 This series, with thanks to our friends at Novartis, we are Talking Melanoma.
This series, with thanks to our friends at Novartis, we are Talking Melanoma.
Over the next eight episodes, our hosts, and guest-host Dermatology Nurse Specialist Selene Daly, will be talking to some great guests like Dr. Patrick Ormond and Dr Osama Salib about the realities of a skin cancer diagnosis and treatment, as well as hearing from patients that are living with and beyond melanoma. We will also hear about some of the supports in place in Ireland and how to cope with a melanoma diagnosis and possible side effects with psycho-oncologist Yvonne O’Meara. We will even have an exclusive interview with Dr Triona McCarthy from the NCCP to discuss how we can all do our part to help reduce our risk of melanoma in the future.
Marie Keating Foundation Talks Cancer is available to stream wherever you listen to podcasts.
Podcast Trailer:
Here's a sneak peek at what to expect from this series of The Marie Keating Foundation Talks Cancer!
Episode One: An Introduction to Melanoma with Dermatology Nurse Specialist Selene Daly
On this weeks episode of “The Marie Keating Foundation Talks Cancer” podcast, our hosts Director of Nursing Services Helen Forristal, Assistant Director of Nursing Bernie Carter and Dermatology Nurse Specialist Selene Daly discuss what melanoma is, the role of a dermatology nurse, how we can all reduce our risk of skin cancer while also sharing some bad sun habits they themselves used to indulge in. Tune in now!
Be sure to follow the podcast on your favourite platform by clicking the icons below and never miss an episode!
Episode Two: Melanoma Diagnosis. the First Steps with Consultant Dermatologist Dr Patrick Ormond
On this week’s episode of the Marie Keating Foundation Talks Cancer podcast, we are chatting to Consultant Dermatologist Dr Patrick Ormond about all things skin. Discussing the signs you should be looking out for on your skin, Breslow depth, the dangers of sunbeds and the process your team goes through to diagnose skin cancer and melanoma. Listen to our full conversation now, and like, follow and subscribe for more.
Episode Three: Talking Melanoma, the treatment plan with Dr Osama Salib and Professor Derek Power
On this episode of the Marie Keating Foundation Talks Cancer Podcast, we will be #TalkingMelanoma treatment with Radio-oncologist Dr Osama Salib and Consultant Oncologist Prof Derek Power. From radiation treatment and immunotherapy to pain management and multidisciplinary teams, in this episode, we will be exploring the treatment options available for those at every stage of a melanoma journey, and the realities of Stage 4 maintenance and care.
Episode Four: Talking Melanoma - the journey from diagnosis to follow up care with melanoma survivor Evelyn O'Neill
On the latest episode of the Marie Keating Foundation Talks Cancer Podcast, our hosts Helen and Bernie chat to melanoma survivor Evelyn O’Neill about what her experience was like being diagnosed and treated for melanoma during a global pandemic. From spotting a dark mole, to going in for surgery without the support of her family and friends, Evelyn’s story is unique as it explores the emotional impact a melanoma diagnosis can have on those affected by the disease. Listen to our conversation today and learn what Evelyn wished she had known about melanoma before she was diagnosed.
Episode Five: Melanoma Myth Busting With Dermatology Nurse Specialist Selene Daly
On this week’s episode of the Marie Keating Foundation Talks Cancer Podcast, our hosts Helen, Bernie and Selene debunk some well known “SunSmart facts” to help us all get to know the truth about protecting our skin. Over the course of this episode, our hosts share some of the bad sun habits they themselves used to believe and correct some misinformation about sunscreen, sunbeds and much more to make sure we all know how to look after our skin from now on. This is an episode you won’t want to miss and is a step by step guide of what NOT to do this summer season.
Episode Six: Talking Melanoma - Living Well With Melanoma, a conversation with Kay Curtin and Shirley McEntee
On the this week’s episode of the Marie Keating Foundation Talks Cancer Podcast, Helen and Bernie have the opportunity to speak to Kay Curtin and Shirley McEntee about living life with metastatic melanoma. From original diagnoses, to progress in the treatment of melanoma over the years and how these incredible women have learned to adapt to their current treatment plans, their journeys are truly inspiring. Listen to their stories and conversations today and find out how Kay and Shirley are now living well with advanced-stage melanoma.
Episode Seven: Talking Melanoma and supportive services with Yvonne OMeara and Stacey Devanney
This week on the Marie Keating Foundation Talks Cancer Podcast, we are chatting to Systemic Psychotherapist and Psycho-social Oncologist Yvonne O’Meara and Senior Social Medical Worker Stacey Devanney about the emotional and financial implications of a melanoma cancer journey. From practical tips on how to manage financially during treatment and the resources available to those on active treatment, to advice and resources on how to manage your emotions and mental health during diagnosis, treatment and late stage palliative care. Tune in to the conversation today and learn about the steps you can take to help support your loved ones that are on a melanoma journey.
Episode Eight: Melanoma Prevention with Dr. Caitriona McCarthy
-
For the final episode of our #TalkingMelanoma series, hosts Bernie and Helen chat to Dr Triona McCarthy about the NCCP’s skin cancer prevention programme, the SunSmart code and the simple steps we can all take to reduce our risk of developing skin cancer in the future. We also explore the importance of looking after younger skin and how we can all do our part to prevent skin cancer in future generations. This episode is full of helpful tips and information and is definitely one to listen to before you head out for your daily stroll.
Don't Cook Yourself

Don't Cook Yourself
Unlike your barbecue, you won’t know you’re burning until it’s too late. It only takes minutes to get cooked by the sun - even in Ireland - and every sunburn dramatically increases your risk of skin cancer. We have one of the highest death rates from melanoma skin cancer in Europe, and the last thing you want is a barbecue to die for.
Ahead of marinades, meat rubs, or cooking sprays, the most essential ingredient for any barbecue under the sun is an SPF 30+ suncream. Making it part of your ritual every time you're getting ready to barbecue will help ensure the only thing that might burn is what's on the grill. 90% of all skin cancer cases are preventable, and it only takes minutes to make sure you're covered.
Anti-Cooking Instructions
 Use an SPF 30+ sunscreen for adults that protects against both UVA and UVB rays
Use an SPF 30+ sunscreen for adults that protects against both UVA and UVB rays- Apply the cream onto any area of your skin that the sun could cook
- Repeat every 2 hours if it’s a long lunch or you’re cooking for a cast of thousands
- For best results, i.e. crucial protection, you should also cover up, wear a hat, BBQ in the shade between 11am and 3pm and wear sunglasses
- Even on a slightly overcast day, 90% of UV rays can get through clouds, so even if you can't see the sun it can still burn you
- If you can’t take the heat, get into the kitchen
Cooking Times
On days when the UV index is moderate to high, your unprotected skin can get cooked by the sun faster than you can cook most BBQ foods. So if you're keeping a close eye on your food, keep yourself well protected too.
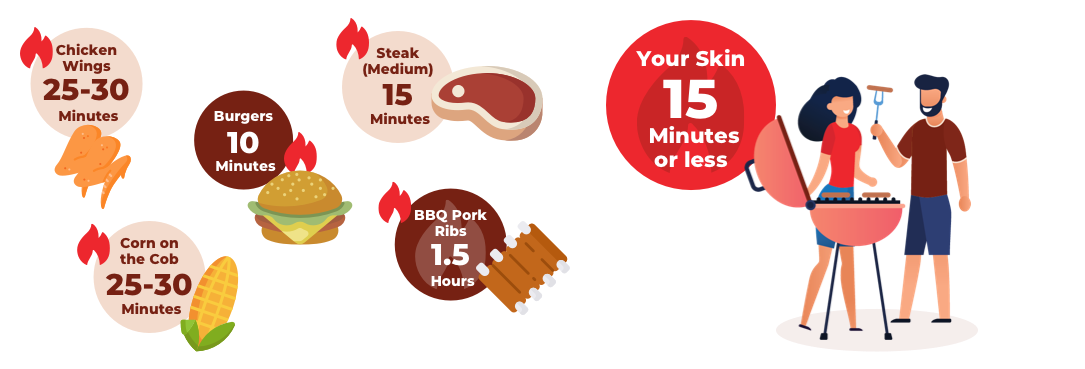
Kindly supported by
![]()
Skin C(h)ancer 2019/2018
![Social – Footballer [square]](https://mariekeating.ie/wp-content/uploads/2020/03/Social-Footballer-square.png)


The Marie Keating Foundation launches new skin cancer campaign, as research reveals Irish men have the highest mortality rate from melanoma skin cancer than anywhere in Europe
The Marie Keating Foundation has launched the latest phase of its skin cancer campaign, Skin C(h)ancer, as worrying figures reveal Ireland has the highest mortality rate for melanoma in Europe, with more men dying from this disease than women.
The cancer foundation’s Skin C(h)ancer campaign is aimed at Irish men who work or spend a lot of time outdoors, particularly sportsmen, farmers and gardeners. The campaign comes off the back of what is believed to be the longest heatwave since 1976 and is a reaction to the startling fact that the incidence of melanoma skin cancer has more than tripled in the two decades from 1994 to 2014.
A recent international skin cancer index has found the death rate from skin cancer in Ireland is higher than in Australia and puts Ireland 14th in the world for susceptibility to skin cancer
Speaking at the campaign launch, in-front of Ireland’s first UV sensitive mural on the Grand Canal, Dublin at Lock 6 Cafe, CEO of the Marie Keating Foundation and malignant melanoma survivor, Liz Yeates said “530 cases of melanoma are diagnosed in Irish men each year, resulting in 88 deaths annually. We’ve launched this campaign to give Irish men a wake-up call and encourage them to take their skin’s health seriously. We are appealing to all men including farmers, gardeners, construction workers and anyone who plays sports outdoors , asking them to not only take their health and safety seriously by wearing high vis vests, gum shields, helmets etc but also to protect their skin from the sun’s harmful UV rays by following the SunSmart code.
She continued “we are activating the campaign on radio, in shopping centres, on social media and in the press, in the hope that we can reach as many people as possible with our message. Our mural looks to highlight the risk that sportsmen are exposed to when they play outdoors all year round – even if the sun isn’t shining. Our message is simple; Don’t take the chance, protect your skin.”
Proudly supported by Novartis as part of their wider Skintervention campaign, the Foundation is urging people to follow these simple steps in the sun:
- Wear sunscreen- with a high factor SPF (50+) and good UVA and UVB protection and apply generously and regularly, ideally every two hours
- Seek shade- especially from 11am to 3pm when UV rays are strongest
- Cover up- with long sleeved clothing and a hat
- Wear sunglasses- with lenses that have UV protection
- Never ever use sunbeds – even just once, as they cause lasting damage
- Check your skin- look for changes in moles and freckles
Also speaking at the launch was Helen Forristal, Director of Nursing Services, the Marie Keating Foundation, who said, “Our research shows that a fifth (20%) of Irish men are not aware of the visible signs of skin cancer, which is worrying as skin cancer is one of the most preventable forms of cancer i f you are careful. You need to be vigilant by knowing your skin-type and checking your skin on a regular basis. Look out for any changes in moles or freckles. If you notice a change in colour, size or shape, bleeding, crusting or itching visit your GP as soon as you can because when melanoma is caught early, it can be treated and the response to treatment can be very effective.”
f you are careful. You need to be vigilant by knowing your skin-type and checking your skin on a regular basis. Look out for any changes in moles or freckles. If you notice a change in colour, size or shape, bleeding, crusting or itching visit your GP as soon as you can because when melanoma is caught early, it can be treated and the response to treatment can be very effective.”
Former Kilkenny hurler and Marie Keating ambassador, Eddie Brennan, said “Having grown up on the family farm and working as a Garda since 1998 I would have spent so much time outside and I would never really have been aware of the dangers or thought much about the harm I was doing to my skin. This campaign has made me think back and realise that for years I was out in the sun whether it was farming or on the mountain bike or on the beat or even on

the hurling pitch, completely exposed. This campaign is spot on in terms of speaking to men - it’s just about education and making sure we are aware of the risks so we can properly protect our skin but often men can be worst at doing this. Small changes like wearing sunscreen, a hat and staying in the shade where possible, will make a big difference and hopefully this campaign will get through with its message.”
In 2019, the Foundation built on the sucess of the Skin C(h)ancer campaign and used their charity partnership with the GAA to promote sun safety to all members of the GAA community both on and off the pitch. At the GAA football quarter final in Croke Park supporters learned more about the importance of being SunSmart when outdoor through SunSmart messaging and for the first time ever, the UV index was presented on the field plasmas for all to see.
There are approximately 11,555 cases of nonmelanoma and 1,194 cases of melanoma skin cancer diagnosed each year in Ireland, and rates continue to rise.
This campaign was proudly supported by Novartis.

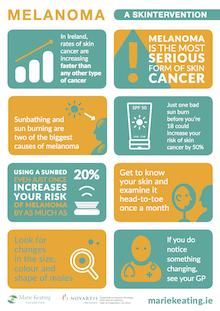
Skintervention 2017
Marie Keating Foundation asks Irish people to be SunSmart
Rates of melanoma, the deadliest form of skin cancer, are rising faster than any other cancer
The Marie Keating Foundation has launched a Skintervention for people in Ireland. Rates of melanoma, the deadliest form of skin cancer, are projected to treble by 2040 but nearly all cases of the disease are preventable. The cancer foundation’s Skintervention campaign is reminding people to be SunSmart as overexposure to UV light, primarily from the sun and sunbeds, causes over 90% of melanoma. Every year, over 900 new cases of melanoma are diagnosed and 163 people die from the disease. Speaking at the launch, Liz Yeates, CEO, the Marie Keating Foundation and a melanoma survivor said, “We are a nation of sun worshippers but we want to remind people that no matter what your age or skin type, it is vital to look after your skin. Just one bad sun burn before you are 18 can increase your chances of skin cancer by half. Using a sunbed, even just once, increases your risk of melanoma by as much as 20%.” To help combat the high levels of melanoma in Ireland, the Marie Keating Foundation is launching a new Skintervention video featuring seven Irish people affected by the disease which can be viewed on www.mariekeating.ie/spotthedifference. In addition, Marie Keating Foundation nurses will be handing out free skin cancer information and free samples of SPF 50 sunscreen throughout the summer, kindly provided by La Roche Posay.
The Marie Keating Foundation is urging people to be SunSmart by following these simple steps:
- Wear sunscreen- with a high factor SPF (Min 30) and good UVA and UVB protection and apply generously and regularly
- Seek shade- especially from 11am to 3pm when UV rays are strongest
- Cover up- with long sleeved clothing and a hat
- Wear sunglasses- with lenses that have UV protection
- Never use sunbeds – even just once, as they cause lasting damage
- Check your skin- look for changes in moles and freckles
Also speaking at the Skintervention launch was Helen Forristal, Director of Nursing Services, the Marie Keating Foundation, who said, “Melanoma is becoming increasingly common in Ireland, and it affects both men and women. However, the good news is you can help prevent it by looking after your skin. You also need to be vigilant by knowing your skin-type and checking your skin on a regular basis. Look out for any changes in moles or freckles. If you notice a change in colour, size or shape, visit your GP as soon as you can because when melanoma is caught early, it can be treated.”
Barbara Brown appears in the Marie Keating Foundation’s Skintervention video. Her sister, Sinead, died from melanoma at the age of 31. Speaking at the launch she said, “Many people think that skin cancer and melanoma are not serious diseases but they can have devastating consequences. If my sister Sinead was here today, she would want you to know that almost all cases of melanoma can be prevented if you just look after your skin by staying out of the sun and wearing high factor SPF. If you know someone who is a sun worshipper, please share this message with them because it could save their life.”
Read our ambassadors stories about their experience with melanoma below
The Skintervention video was created DDFH&B with the kind support of Novartis.

Spot the Difference 2016
Melanoma: Get to Know Your Skin
What is melanoma?
Melanoma is a type of skin cancer that forms in the cells that make melanin. It starts on the normal skin surface and looks like a mole. If melanoma is diagnosed early there is a better chance of cure. Early detection saves lives. Melanoma is the most serious type of skin cancer. It affects both men and women and can affect people of all ages. Over 1,000 cases of melanoma are diagnosed in Ireland each year.
Melanoma Infographics
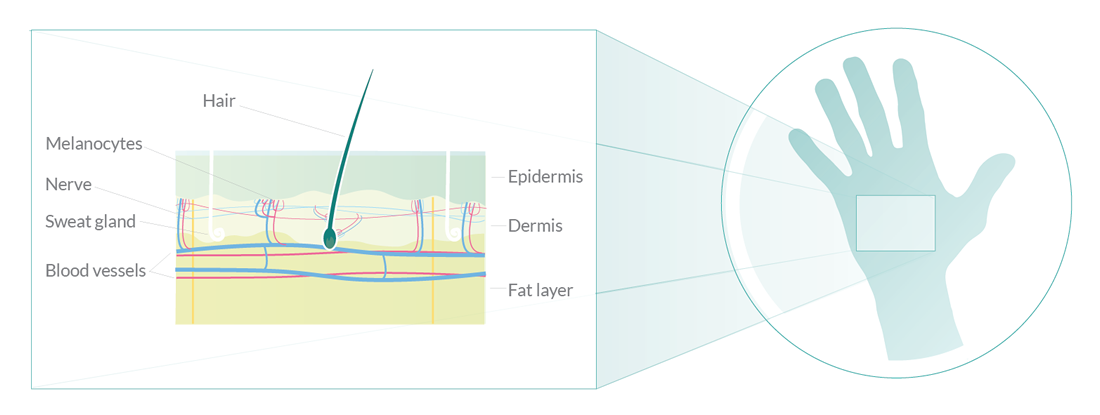
Your Skin
The skin is an organ, like your heart and kidneys. The skin is the biggest organ in the body. Your skin does several important jobs such as acting as a barrier and protecting everything inside your body. The skin is made up of two main layers: the epidermis on the outside and the dermis underneath. New cells are made in the deep layers of the epidermis and are pushed towards the surface. The epidermis is mainly made up of flat, scale-like cells called squamous cells. These cells make a substance called keratin, a tough, waxy substance that helps to make the skin strong enough to protect the body. At the base of the epidermis are cells called melanocytes which make a pigment called melanin. This pigment gives your skin its colour and protects it from ultraviolet (UV) rays in sunlight. Under the squamous cells are round cells called basal cells. These cells constantly divide to form new keratin-producing cells to replace the ones that wear off the skin’s surface.
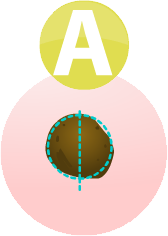
If you draw a line through a melanoma, the two sides will not match
The border of an early melanoma tends to be uneven. The edges may be scalloped or notched.

Most healthy moles are all one colour. A mole with a number of different shades of brown, black or tan is a warning sign. Melanomas may also be blue, red or some other colour
Melanomas are usually larger in size than the rubber at the top of a pencil (¼ inch or 6mm)
Any change in shape, colour, size, elevation (height), or any other trait, or a new symptom like bleeding, itching or crusting is a warning sign
Dr Ormond on the ABCDEF method examining moles.
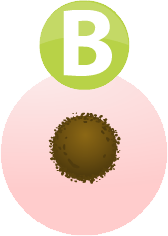
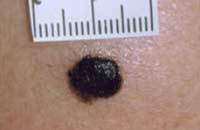 The photo shows a very dark mole. Darkening is one possible sign that a mole is becoming cancerous and could be a melanoma. This mole is about a centimetre across.
The photo shows a very dark mole. Darkening is one possible sign that a mole is becoming cancerous and could be a melanoma. This mole is about a centimetre across.
 The photo shows the irregular outline of a melanoma. Normal moles are usually much rounder, with smooth borders.
The photo shows the irregular outline of a melanoma. Normal moles are usually much rounder, with smooth borders.
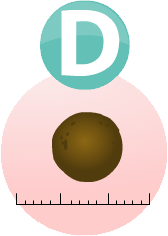
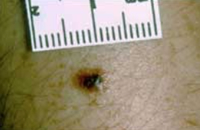
 The photo shows a mole that has an area of inflammation around it. The inflamed area is about 7 millimetres at its widest but you can see that the original mole is much smaller than that. Inflammation is another sign that a mole may be developing into a melanoma and needs to be checked out by a doctor.
The photo shows a mole that has an area of inflammation around it. The inflamed area is about 7 millimetres at its widest but you can see that the original mole is much smaller than that. Inflammation is another sign that a mole may be developing into a melanoma and needs to be checked out by a doctor.
 This is an image of a very small melanoma. It is only about 4 or 5 millimetres across. But you can see clearly that it is not the same colour throughout. It also has an irregular shape. Irregular colour and shape are signs that should be checked by a doctor.
This is an image of a very small melanoma. It is only about 4 or 5 millimetres across. But you can see clearly that it is not the same colour throughout. It also has an irregular shape. Irregular colour and shape are signs that should be checked by a doctor.
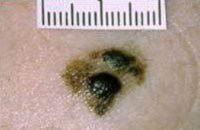 The picture shows clearly a melanoma that is spreading out from a normal mole. If you have a mole that has changed in this way, you should see your doctor as soon as possible.
The picture shows clearly a melanoma that is spreading out from a normal mole. If you have a mole that has changed in this way, you should see your doctor as soon as possible.
Causes
The exact cause of melanoma is not known but there are certain things that increase your chances of getting the disease. These are called risk factors. If you have one or more risk factors for melanoma, it does not mean that you will definitely get the disease, but it does mean that you should be especially careful about monitoring your skin for any changes, you should be SunSmart, and you should go to your GP straight away if you notice any changes.
The more moles you have on your body, the higher your risk of melanoma. You should be very careful about exposing yourself to the sun and should keep an eye on all your moles.
People who have had sunburn are twice as likely to get melanoma as those who have not. The risk is higher if you have had sunburn several times in your life.

UV light comes from the sun. Over exposure to sunlight can cause patches of rough, dry skin called solar keratoses, which increases your risk of melanoma by up to 4 times.

If you have a family history of any type of skin cancer then your risk increases.

Using a sunbed, even just once, increases your risk of melanoma by 20%. Using a sunbed before the age of 35 increases your risk by almost 60%. Never, ever use sunbeds.

People who are exposed to strong sunlight now and then, for example if you live in Ireland and holiday in a hot country, are more at risk of melanoma than people who are continuously exposed to sunlight.
A very rare type, called a congenital giant melanocytic naevus, can develop into a melanoma. They are very common on the buttock.
![]()
Fair skinned people born in a hot country, for example Australia, have a higher risk than people who went to live in a hot country as a teenager or people with similar skin colouring who live in cooler climates.
 Apply the cream 20-30 minutes before going out into the sun. Apply thickly and evenly every 2 hours no matter how high its protection. Apply the equivalent of a shot glass full of sunscreen to each limb and to your body and about half this much to your face. Always reapply after swimming or perspiring. Remember no sunscreen gives 0% protection from the sun.
Apply the cream 20-30 minutes before going out into the sun. Apply thickly and evenly every 2 hours no matter how high its protection. Apply the equivalent of a shot glass full of sunscreen to each limb and to your body and about half this much to your face. Always reapply after swimming or perspiring. Remember no sunscreen gives 0% protection from the sun.
 Choose a sunscreen that has good protection against UVA rays as well as a high SPF. This is because both UVB and UVA rays can cause skin cancer. In Ireland, the level of UVA protection might be shown in one of two ways
Choose a sunscreen that has good protection against UVA rays as well as a high SPF. This is because both UVB and UVA rays can cause skin cancer. In Ireland, the level of UVA protection might be shown in one of two ways
- Star rating
- A symbol with the letters UVA inside a circle
 ...as this is when the sun's rays are strongest. This applies all year round, not just in summer. It is important to remember that the sun's rays are present even on a cloudy day.
...as this is when the sun's rays are strongest. This applies all year round, not just in summer. It is important to remember that the sun's rays are present even on a cloudy day.
 Clothing should be dark and tightly woven and cover your arms and legs. Wear a broad-brimmed hat that provides lots of shade. Remember to protect your eyes too by wearing sunglasses. Choose a wraparound pair that give UV protection. Check the sunglass tags to ensure that they give good protection. You can look out for these quality marks:
Clothing should be dark and tightly woven and cover your arms and legs. Wear a broad-brimmed hat that provides lots of shade. Remember to protect your eyes too by wearing sunglasses. Choose a wraparound pair that give UV protection. Check the sunglass tags to ensure that they give good protection. You can look out for these quality marks:
- European Standard EN1836
- British Standard BS 27241987
 Sunbeds are not a safe alternative to tanning outdoors. The intensity of some of the UV rays they give off can be 10 to 15 times higher than that of the midday sun. Using a sunbed, even just once, increases your risk of melanoma by 20%. Using a sunbed before the age of 35 increases your risk by almost 60%.
Sunbeds are not a safe alternative to tanning outdoors. The intensity of some of the UV rays they give off can be 10 to 15 times higher than that of the midday sun. Using a sunbed, even just once, increases your risk of melanoma by 20%. Using a sunbed before the age of 35 increases your risk by almost 60%.
What to do if your mole changes
Go to your GP
 The signs of melanoma are that a mole has changed in size, shape and colour or it looks red and inflamed, oozes, bleeds, is crusty or is itchy or painful. If you notice any of these changes, you should see your GP without delay.
The signs of melanoma are that a mole has changed in size, shape and colour or it looks red and inflamed, oozes, bleeds, is crusty or is itchy or painful. If you notice any of these changes, you should see your GP without delay.
Your GP will look at the mole and ask you what you have noticed about it. He or she will examine your skin and if they think that your mole looks as if it might be melanoma, they will arrange for you to see a skin specialist, called a dermatologist. You should be seen within 2 weeks.
Seeing a dermatologist
When you have your appointment with the dermatologist, they will examine your skin again. He or she may ask you about your family history of melanoma as well as other questions about your health and especially your skin.
The dermatologist might use two different tests to establish if you have melanoma:
- A skin exam, which is also called a dermatoscopy
- An excision biopsy
Skin Exam/ Dermatoscopy
A dermatoscopy may be used by the dermatologist to help make the initial diagnosis. The doctor uses an instrument called a dermatoscope to closely examine the suspicious area on your skin. The doctor puts some oil on to your skin and then holds the dermatoscope in their hand, a bit like a magnifying glass. This can magnify the area by up to 10 times so that the doctor can see it very clearly. It is completely painless.
Excision biopsy
A biopsy means taking a sample of cells and looking at them under a microscope. However, in the case of a suspicious mole, instead of taking just a sample, the dermatologist or a plastic surgeon will take the entire mole. This is called an excision biopsy.
When you go to have your mole removed, the nurse or doctor will ask you to lie down on a couch in the treatment room. First you have an injection of local anaesthetic into the area close to the mole to numb it. The doctor then cuts out the mole. He or she will also remove 2mm of tissue around the mole to help ensure that, if the mole is cancerous, that they have removed all of the cancerous cells. The mole is then sent to the laboratory for close examination under a microscope. You may need to have a few stitches in the place where the mole was removed. These will usually dissolve after a few days, or you may need to go back to the doctor's office to have them removed.
You may get your biopsy results at the hospital or at your GP surgery. If the mole contained any cancerous cells you may need to have more tests. If not, you will not need any more treatment. Your doctor will discuss this with you.
If your mole contained cancerous or precancerous cells, a tissue specialist (histopathologist) will look at the biopsy tissue very closely in the laboratory. Your doctor will ask you to go into hospital for an operation to take away more tissue. This aims to remove any abnormal cells that may have been left behind in the area close to the melanoma. It reduces the chance of the melanoma coming back in the future. The operation is called a wide local excision. You can read more about this in the Surgery section under the Treatment part of this website.
Further tests
If you are found to have melanoma, your doctor will check how deep the melanoma is. The depth of the melanoma in the skin affects how likely it is to come back and whether it may spread. If you have early stage melanoma that is only in the surface layers of the skin, the melanoma is very unlikely to have spread anywhere else. You will not need to have further tests.
If you do need further tests, your medical team will discuss these with you. These tests may include a sentinel lymph node biopsy, CT scan, ultrasound scan, MRI scan, PET scan with CT, and/or a bone scan.
Out and About
The Marie Keating Foundation mobile information units are helping people across Ireland to Spot the Difference. Throughout the summer, the mobile information units, each staffed by a registered nurse, will be visiting schools, community centres, shopping centres, and offices to give people free advice about skin cancer. The Marie Keating Foundation nurses will be handing out free samples of SPF 50 sunscreen, kindly provided by La Roche Posay, alongside information on how to prevent and detect skin cancer at its earliest stages.
If you would like to arrange for the Marie Keating Foundation mobile units to visit your community group, school or college, please contact us. This is a completely free service and the Foundation would be delighted to help your organisation learn how to Spot the Difference.

Skin Cancer Resources
To read a copy of the information you should know leaflet, click here.
To download a copy of our advanced melanoma booklet, click here.
Donate to Marie Keating
We hope you found this information useful. The Marie Keating Foundation offers all of our services for free. Help support people at every step of a cancer journey by making a donation today.
DONATE