
- Facts about skin cancer
- What is the skin?
- Types of skin cancer - non-melanoma
- Risks and causes of skin cancer
- UV - What You Should Know
- Skin cancer prevention
Facts about skin cancer
- Skin cancers are divided into two main types: melanoma and non-melanoma
- Non-melanoma skin cancer is the most common cancer in Ireland, with melanoma being the fourth most common
- There are over 11,736 non-melanoma skin cancers and over 1,156 melanomas diagnosed every year
- The number of people diagnosed rises each year
- More men than women are diagnosed with non-melanoma skin cancer
- Being SunSmart is vital to preventing skin cancer
For information on melanoma skin cancer, visit our melanoma page.
What is the skin?
The skin is an organ, like your heart and kidneys. The skin is the biggest organ in the body and does several important jobs such as acting as a barrier and protecting everything inside your body.
The skin is made up of two main layers: the epidermis on the outside and the dermis underneath. New cells are made in the deep layers of the epidermis and are pushed towards the surface. The epidermis is mainly made up of flat, scale-like cells called squamous cells. These cells make a substance called keratin, a tough, waxy substance that helps make the skin strong enough to protect the body. At the base of the epidermis are cells called melanocytes which make a pigment called melanin. This pigment gives your skin its colour and protects it from ultraviolet (UV) rays in sunlight. Under the squamous cells are round cells called basal cells. These cells constantly divide to form new keratin-producing cells to replace the ones that wear off the skin’s surface.
 Different types of skin cancer
Different types of skin cancer
There are different types of skin cancer. The type of skin cancer depends on the skin cells that are affected.
- If the cells affected are the basal or squamous cells, it is called non-melanoma skin cancer (NMSC)
- If the melanocytes are affected, it is called melanoma skin cancer. Read about melanoma here.
Skin cancer (non-melanoma)
Non-melanoma skin cancer is the most common cancer in Ireland. There are several different types of non-melanoma skin cancer. The most common types are basal cell cancer (BCC) and squamous cell cancer (SCC). Sometimes these cancers are called ’carcinomas.’
Basal cell cancer (BCC)
The most common type of skin cancer, this develops from basal cells which are in the deepest layer of the epidermis and around the hair follicle. It develops mostly in areas of skin exposed to the sun, including parts of the face such as the nose, forehead and cheeks. It can also develop on your back, particularly in men, or lower legs. It is most often diagnosed in people of middle or old age.
Basal cell cancer may start as a small lump that gets bigger slowly over months and years. The edges usually have a shiny or pearly look and the middle is usually sunken. Sometimes the middle becomes crusty or an ulcer develops. It usually will not hurt unless knocked but it can be itchy and may bleed if scratched.
It is very rare for basal cell skin cancer to spread to another part of the body to form a secondary cancer. It is possible to have more than one basal cell cancer at any one time. Having had one increases your risk of getting another.
Squamous cell cancer (SCC)
This cancer begins in cells called keratinocytes, which are the cells nearest the surface of your skin, lying just above the basal cells. Squamous cell cancer most often develops in areas that have been exposed to the sun, including parts of the head, neck, and on the back of your hands and forearms. Rarely, it can develop around your vulva or anus. It can also develop in scars, areas of skin that have been burnt in the past or areas of skin that have been ulcerated for a long time.
Squamous cell skin cancer can look like a crusty, scaly ulcer. Or it may be bumpy and hard and develop into an ulcer. This type of cancer is generally faster growing than basal cell cancer though it does not usually spread.
Risks and causes of skin cancer
- Sunbeds- Using sunbeds greatly increases your risk
- Skin types- People who have fair skin; lots of moles or freckles; or red or fair hair have a greater risk
- Age- Non-melanoma skin cancers develop very slowly. As you get older you have more time to build up sun damage. However, young people can get skin cancer too
- Having had skin cancer before- If you have had a non-melanoma skin cancer, you have about a 10 times higher risk of a second non melanoma skin cancer
- Other skin conditions-People with certain skin conditions or skin treatments can be more likely to develop skin cancer. These include: psoriasis, scarring; solar keratosis; and atopic dermatitis
- Family history- If someone in your family has had any type of skin cancer, this increases your risk
- Sun exposure- Most skin cancers are caused by sun exposure, either long-term or short periods of intense sun exposure and burning, perhaps while on holiday. Remember even on a cloudy day, UV rays can be strong enough to cause skin damage that can lead to skin cancer
UV – What you should know
UV or Ultraviolet Radiation is a form of electromagnetic radiation that comes from the sun and man-made sources like tanning beds and welding torches. This source of radiation is incredibly harmful to unprotected skin and can greatly increase a person's risk of developing skin cancer.
The two main types of UV that affect the skin are UVA waves and UVB. These types of radiation are emitted from the sun and can cause long term skin damage such as pigmentation and wrinkling if the skin is left unprotected. These types of rays are also known the damage the skins DNA structure, drastically increasing a person's risk of developing skin cancer later in life. UV rays are responsible for sunburns and as we know, even one bad sunburn can damage your skin and increase in your risk of developing skin cancer in the future.
The UV Index:
The Global Solar UV index is a scale developed by the World Health Organisation to help measure the UV radiation level on the surface of the Earth, and give an indication of the potential for skin damage on any particular day.
The UV index helps us to determine how high the risk is each day so we can plan ahead to protect our skin from damage throughout the day.
The scale is based on 1 to 11+ number scale and as the UV rating climbs, so does your risk.
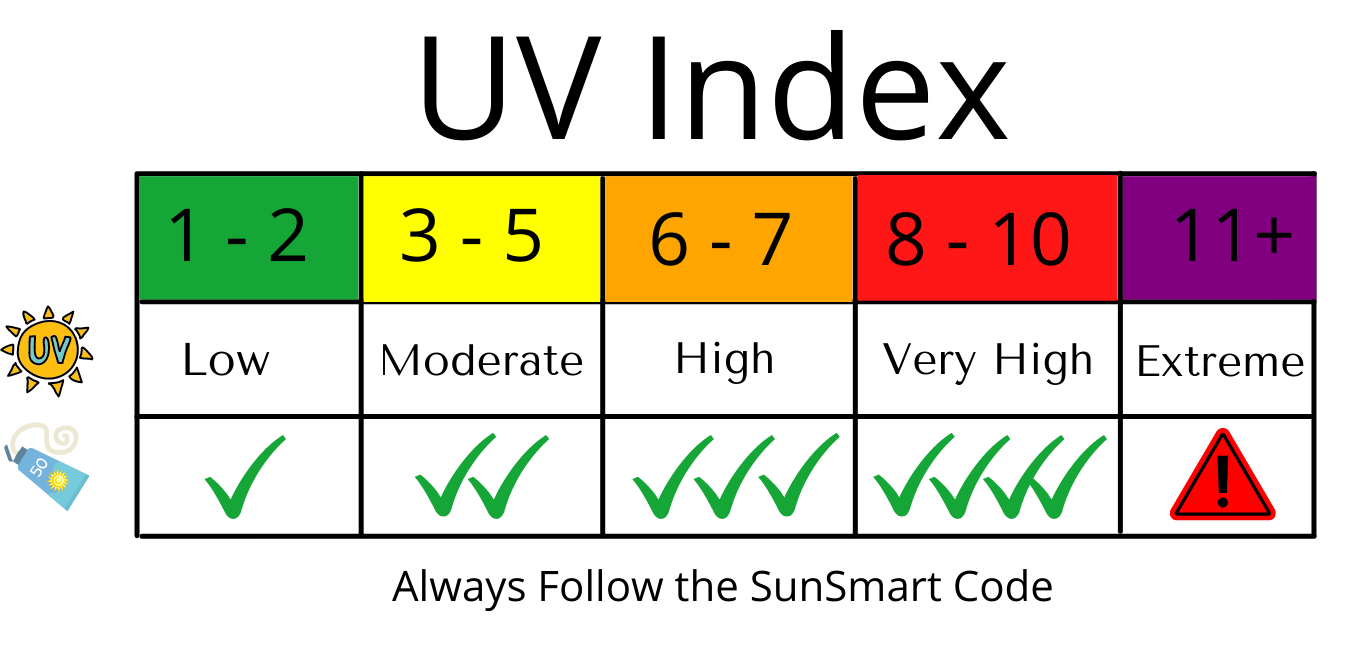
Remember, protecting your skin from harmful radiation is important all year round, not just in the summer. UV rays can penetrate the clouds surface and damage your skin even when the sun isn’t visible so it’s essential to make being SunSmart and checking the UV Index in your area, a part of your daily routine.
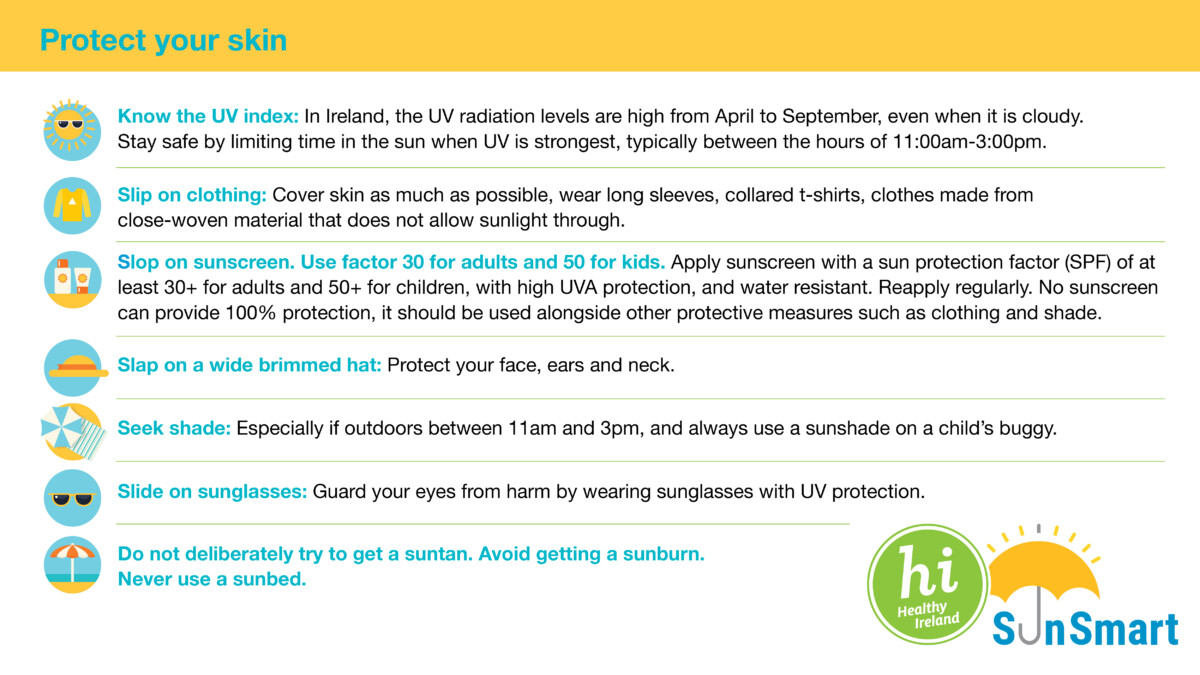
5 S’s of being SunSmart:
While non-melanoma skin cancer is Ireland’s most common forms of cancer, it is also one of the most preventable forms of cancer.
The National Skin Cancer Prevention Plan developed by the HSE and the National Cancer Control Programme is designed to help you reduce your risk of skin cancer while spending time outdoors. To be SunSmart and prevent skin cancer, it is recommended that each day, we all follow the 5 S’s of the SunSmart code, which are:
- Slop on sunscreen with a good UV rating and factor 30+ - by wearing sunscreen every day, you are protecting your skin no matter the weather
- Slip on sun protective clothing – When spending time outdoors it's important to wear clothes that cover your skin such as hats and anything with long sleeves, to help reduce the impact of the suns rays on unprotected skin
- Slap on a wide brimmed hat- Wearing a hat can help to protect the skin on your face and neck from direct sun exposure and will help to reduce your risk of skin cancer
- Slide on sunglasses – protect your eyes from the suns glare by sliding on a pair of sunglasses with UV protection
- Seek shade – This is especially important if you are outdoors between the hours of 11am and 3pm when the sun is at it's peak
What skin cancer can look like
- A spot or sore that does not heal within 4 weeks
- A spot or sore that itches, hurts, is scabbed or crusty, or bleeds for more than 4 weeks
- Areas where the skin has broken down (an ulcer) and doesn't heal within 4 weeks, and you can't think of a reason for this change
Basal cell skin cancers look like a small, slow-growing, shiny, pink or red lump. They can also look like red scaly patches. If left, basal cell skin cancers tend to become crusty, bleed, or develop into an ulcer. They are most common on the face, scalp, ears, hands, shoulders and back.
Squamous cell skin cancers are usually pink lumps. They may have hard or scaly skin on the surface. They are often tender, but not always. They can bleed easily and develop into an ulcer. They are most common on the face, neck, lips, ears, hands, shoulders, arms and legs.
 Diagnosing skin cancer
Diagnosing skin cancer
If you notice a change on your skin that does not heal over 4 weeks and that you cannot explain, visit your GP. He/she may refer you to a skin specialist called a dermatologist who will give you a skin exam where they will look at your skin under a special magnifying glass. The dermatologist or a plastic surgeon may also remove the mole or affected skin, so that the cells can be looked at under a microscope. This is called a biopsy. During a biopsy, at least 2-5 mm of normal looking skin will be removed as well to ensure that all unusual tissue is removed. A biopsy is usually performed under local anaesthetic.
Depending on what the doctor sees when he or she looks at biopsy tissue under the microscope, you may not need any further treatment. If you do, the doctor will discuss this with you.
Visit Spot the Difference
For a copy of the Marie Keating Foundation's skin cancer information leaflet, click here.
Donate to Marie Keating
We hope you found this information useful. The Marie Keating Foundation offers all of our services for free. Help support people at every step of a cancer journey by making a donation today.
DONATE
